Pericardiocentesis is a procedure to remove fluid that has built up in the sac around the heart (pericardium). The fluid is drained with a needle and flexible tube (catheter).
Why pericardiocentesis is done
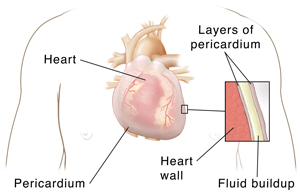
A fibrous sac surrounds the heart. The sac is called the pericardium. It’s made of two thin layers with a small amount of fluid between them. The fluid helps cushion the two layers as they rub against each other when the heart beats.
Many types of medical conditions can cause fluid to build up in this sac. This is called pericardial effusion. The fluid buildup can cause shortness of breath and chest pain. This may be treated with medicines. In other cases, this fluid buildup is life-threatening and needs to be drained right away.
Pericardiocentesis is done to drain the fluid around the heart. And it can help diagnose the cause of the extra fluid.
How pericardiocentesis is done
Your procedure will be done by a cardiologist, or a cardiac surgeon. These are health care providers who specialize in diseases of the heart. The provider will put the needle through the skin below the breastbone. They will guide the needle to the fluid in the pericardial sac. This is frequently done with the help of an echocardiogram. Or it may be done with live X-ray imaging called fluoroscopy. Once the needle is in the right area, the provider will put a catheter in that place. They will then remove the needle. Fluid will drain out through the catheter. The catheter will be removed when enough fluid has drained. The catheter may stay in place for several hours or days. Or it may be removed sooner.
Risks of pericardiocentesis
All procedures have some risks. Risks of pericardiocentesis include:
-
Puncturing of the heart, which may require surgery to repair.
-
Excess bleeding, which might press on the heart and affect its function.
-
Air in the chest cavity.
-
Infection.
-
Return of the fluid around the heart.
-
Need for a repeat procedure.
-
Abnormal heart rhythms (arrhythmias) that can cause death in rare cases.
-
Heart failure with fluid in the lungs (rare).
Your own risks may vary according to your age, your general health, and the reason for your procedure. They may also vary depending on the structure of your heart and pericardium, and the amount of fluid. Talk with your provider about which risks apply most to you.